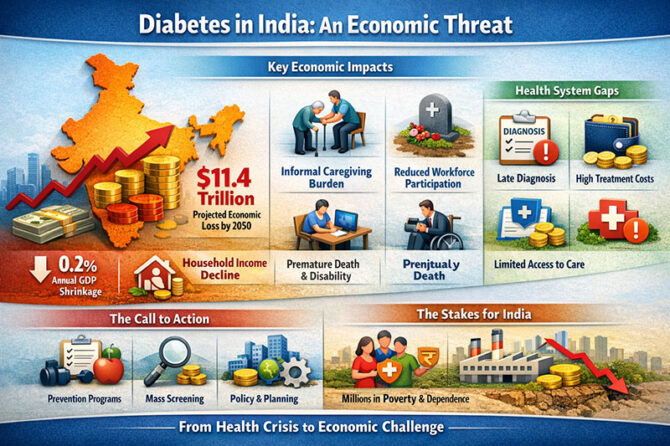
Diabetes in India has crossed a critical threshold. It is no longer merely a clinical problem managed within outpatient clinics and hospitals; it has evolved into a macroeconomic risk capable of reshaping national productivity, household incomes, and long-term development. A recent global modelling study reported by The Times of India estimates that diabetes will cost India an astonishing $11.4 trillion between 2020 and 2050, placing the country second globally—just behind the United States and ahead of China
What makes this figure especially sobering is not the direct medical expenditure alone. The study adopts a health-augmented macroeconomic model, comparing a future in which diabetes continues unabated with a hypothetical counterfactual world without diabetes. The difference between these two futures—lost GDP—captures the true cost of the disease. This includes premature mortality, disability, reduced labour productivity, early exit from the workforce, diversion of household savings into long-term care, and the often-ignored economic value of unpaid family caregiving.
As the TOI analysis underscores, informal caregiving emerges as the dominant driver of economic loss in South Asia, accounting for nearly 90% of the total burden in some scenarios. This hidden cost rarely appears in government budgets, yet it quietly drains household incomes and reduces labour participation, particularly among women. In effect, diabetes does not disable one individual—it partially removes entire families from the productive economy.
An international perspective highlights a crucial contrast. In high-income countries, nearly 40% of diabetes-related economic damage arises from treatment costs—expensive drugs, hospitalisation, and advanced therapies. In India and other low- and middle-income countries, this proportion falls to around 15%. This does not indicate lower disease severity; rather, it reflects under-diagnosis, delayed treatment, and limited access to continuous care. As the study notes, people in poorer countries often “pay not with money, but with lost years of work, disability, and dependence on family members.”
India’s vulnerability is amplified by scale. With approximately 90 million adults currently living with diabetes, the country now accounts for more than a quarter of the world’s diabetic population. Even modest per-patient costs multiply into enormous national losses when applied across such numbers. The modelling suggests that diabetes alone erodes about 0.2% of India’s cumulative GDP over three decades, before the full effect of informal caregiving is included. Over time, this acts like a persistent tax on economic growth.
The drivers of this epidemic are well documented in the TOI article. Dietary transitions toward polished rice, refined wheat, packaged foods, and sugary beverages have raised glycaemic load across populations. Urbanisation and desk-based work have displaced daily physical activity, while long screen hours and disrupted sleep patterns further worsen metabolic risk. Importantly, the article highlights a biological vulnerability among South Asians, who develop insulin resistance and central obesity at lower body-mass indices than many Western populations.
Health-system gaps compound these risks. Routine screening remains uneven across states, diagnosis is often delayed by several years, continuity of primary care for chronic disease is weak, and high out-of-pocket costs discourage follow-up. Nearly half of all people with diabetes globally remain undiagnosed, and about 90% of these undetected cases are in low- and middle-income countries. When these individuals eventually enter care—often after complications develop—the economic damage is already irreversible.
From an advisory standpoint, the most striking conclusion of the TOI-cited research is that prevention is no longer optional—it is fiscally essential. Evidence reviewed in the study suggests that up to 90% of type-2 diabetes is preventable through sustained lifestyle interventions: regular physical activity, healthier diets, weight control, and avoidance of tobacco. Early detection through large-scale screening can preserve not only lives, but also economic independence and workforce participation.
As one implicit message from the international modelling community makes clear: “Chronic diseases like diabetes are not just health expenditures; they are growth suppressors.” For India, where informal employment dominates and social safety nets are limited, every untreated diabetic today represents a future loss of labour, a caregiver pulled out of paid work, and a compounding drag on national productivity.
The policy implication is unavoidable. Diabetes prevention and early management must move out of siloed health programmes and into the domains of economic planning, labour policy, urban design, food systems, and education. As the TOI analysis succinctly frames it, diabetes is no longer just a public-health crisis—it is a development challenge with trillion-dollar consequences.
Dr. Prahlada N.B
MBBS (JJMMC), MS (PGIMER, Chandigarh).
MBA in Healthcare & Hospital Management (BITS, Pilani),
Postgraduate Certificate in Technology Leadership and Innovation (MIT, USA)
Executive Programme in Strategic Management (IIM, Lucknow)
Senior Management Programme in Healthcare Management (IIM, Kozhikode)
Advanced Certificate in AI for Digital Health and Imaging Program (IISc, Bengaluru).
Senior Professor and former Head,
Department of ENT-Head & Neck Surgery, Skull Base Surgery, Cochlear Implant Surgery.
Basaveshwara Medical College & Hospital, Chitradurga, Karnataka, India.
My Vision: I don’t want to be a genius. I want to be a person with a bundle of experience.
My Mission: Help others achieve their life’s objectives in my presence or absence!
My Values: Creating value for others.
Reference:
- https://timesofindia.indiatimes.com/toi-plus/health/the-11-4-trillion-disease-how-diabetes-is-quietly-bleeding-indias-economy/articleshow/127834616.cms
- Yesudian CAK, Grepstad M, Visintin E, Ferrario A. The economic burden of diabetes in India: A review of the literature. Global Health. 2014;10(1):80. This review highlights direct and indirect cost components, including productivity loss and caregiver time, underscoring methodological challenges in cost estimation.
- Kumar A, India towards diabetes control: Key issues. Indian J Med Res. 2013;137(4): pp.xxx-xxx. Discusses the long-term socio-economic consequences of rising diabetes prevalence in India and its burden on households.
- Nagarathna R, Cost of Management of Diabetes Mellitus: A Pan India Study. J Clin Diagnostic Res. 2021;15(10): OCxx-OCxx. Presents data on direct and indirect expenditures borne by Indian households treating diabetes.
- The $11.4-trillion disease: How diabetes is quietly bleeding India’s economy. The Times of India (TOI Plus). Feb 1, 2026. Reports a global modelling study published in Nature Medicine estimating that diabetes will cost India an estimated US$11.4 trillion between 2020 and 2050, driven by lost GDP and caregiving burden.
- Diabetes – A silent drain on India’s GDP. Mumbai Mirror. Feb 3, 2026. Summarises the same Nature Medicinestudy, noting that diabetes’ economic toll far exceeds treatment costs, emphasising labour and productivity loss.
- Oberoi S, Kansra P. Economic menace of diabetes in India: a systematic review. Glob Health. 2020;16:xx. Reviews direct and indirect costs of diabetes across Indian contexts, including household economic burden.
- B Bansode. Economic burden of diabetic patients in India: A review. Procedia Social and Behavioral Sciences. 2019;xx:xx–xx. Reviews direct and indirect cost categories (medical, non-medical, productivity loss) across Indian regions.
- Nanda M, Sharma R. Financial burden of seeking diabetes mellitus care in India: Evidence from a Nationally Representative Sample Survey. Health Econ Public Policy. 2023;xx(xx):xx–xx. Reports extensive out-of-pocket expenditures and catastrophic health spending among households with diabetes.
- Diabetes in India (Wikipedia, last updated). Provides prevalence estimates and historical growth in the number of people living with diabetes in India, contextualising the scale of the public health challenge.
- Encyclopedia/WHO resources on chronic diseases and economic burden (e.g., Non-communicable diseaseoverview). Discusses the broader global economic impacts of chronic conditions such as diabetes, including productivity losses and national income effects.

















Leave a reply