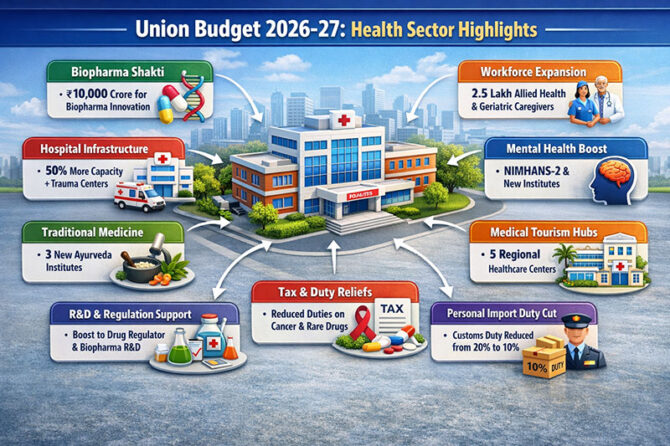
The Union Budget 2026–27 signals a decisive shift in India’s health policy—from incremental funding to system-level capability building. Rather than treating healthcare as a social expenditure alone, the budget positions it as a strategic economic sector, spanning biopharma, workforce, infrastructure, regulation, and global services. This approach aligns India more closely with health-led growth models seen in countries such as the US, Germany, South Korea, and Singapore.
As the World Health Organization (WHO) has repeatedly emphasized, “Health systems are not a cost; they are an investment in human capital and economic resilience” (WHO, World Health Report). The 2026–27 budget reflects this philosophy with unusual clarity.
1. Biopharma Shakti: From Pharmacy of the World to Innovation Hub
The ₹10,000 crore Biopharma Shakti scheme over five years is arguably the most consequential announcement. India has long been a global leader in generic drugs, vaccines, and contract manufacturing. However, value capture has remained limited due to weak presence in novel biologics, biosimilars, cell and gene therapy, and translational research.
This scheme explicitly targets that gap—supporting biotech startups, translational research, manufacturing scale-up, and regulatory-grade innovation. The strategic intent mirrors the US NIH–DARPA–BARDA ecosystem, which converted federal R&D funding into biotech dominance.
As Dr. Francis Collins, former Director of the US National Institutes of Health, noted in published lectures: “Public investment in biomedical research is the seed corn from which entire innovation ecosystems grow.” India is now planting that seed systematically.
Advisory insight:
For Indian hospital groups, diagnostics chains, and medical colleges, this opens partnership opportunities in clinical trials, bio-banks, real-world evidence generation, and translational research—areas historically underutilized in India.
2. Workforce Expansion: Solving Healthcare’s Structural Bottleneck
The planned training of 1 lakh Allied Health Professionals (AHPs) and 1.5 lakh NSQF-aligned caregivers addresses one of India’s most critical constraints: the mismatch between infrastructure and skilled manpower.
International experience is instructive. In the UK’s NHS and Germany’s hospital system, allied professionals account for over 60% of direct patient-care hours. India, by contrast, has relied excessively on doctors and nurses, creating cost inflation and burnout.
As Atul Gawande observed in Being Mortal: “Healthcare does not fail because of lack of doctors alone; it fails because systems forget the people who actually make care work.”
Advisory insight:
Hospitals that integrate AHP-led care models—radiology technologists, anaesthesia technicians, rehabilitation therapists, geriatric caregivers—will see immediate gains in productivity, patient throughput, and margins.
3. District Hospitals and Trauma Care: Infrastructure Where It Matters
A 50% capacity expansion in district hospitals, combined with new Emergency and Trauma Care Centres, represents a quiet but powerful correction. India’s tertiary hospitals are overcrowded not because of demand alone, but because district-level care has been structurally underpowered.
Countries such as Japan and France demonstrate that strong secondary hospitals reduce tertiary overload by up to 30–40%. The budget’s focus on district hospitals reflects this global lesson.
Advisory insight:
Private healthcare operators should anticipate partnerships—PPP models, diagnostics outsourcing, emergency services management—around district hospitals, particularly in Tier-2 and Tier-3 regions.
4. Regional Medical Hubs and Medical Tourism
The proposal for five regional medical hubs integrating diagnostics and rehabilitation directly supports India’s ambition in medical tourism. Unlike earlier efforts focused only on tertiary surgery, this model emphasizes continuum of care, a critical expectation for international patients.
As Michael Porter of Harvard Business School wrote in Redefining Health Care: “Value in healthcare is created across the full cycle of care, not at isolated points of intervention.”
Advisory insight:
States and hospital chains that build bundled care pathways—treatment, rehab, long-stay recovery, tele-follow-up—will dominate inbound medical travel.
5. Ayurveda and Integrative Medicine: Formalizing What Already Exists
The establishment of three new All India Institutes of Ayurveda moves traditional medicine from the margins toward structured, evidence-oriented integration. Globally, integrative medicine models are expanding—most notably at the Mayo Clinic and Cleveland Clinic, where lifestyle and complementary therapies coexist with modern medicine under evidence-based frameworks.
Advisory insight:
Hospitals that selectively integrate Ayurveda, wellness, and rehabilitation—especially in chronic disease and geriatric care—can unlock differentiated offerings without diluting clinical rigor.
6. Mental Health Expansion: Infrastructure Meets Social Reality
Plans for NIMHANS-2 and expanded mental health institutes in Ranchi and Tezpur reflect recognition of India’s growing mental health burden. The Lancet Commission on Global Mental Health has highlighted that untreated mental illness costs economies nearly 4% of GDP through lost productivity.
As the Commission notes: “There is no health without mental health.”
Advisory insight:
Mental health is rapidly becoming a core service line—not an auxiliary one. Tele-psychiatry, community mental health clinics, and employer-linked programs will see accelerated growth.
7. Regulatory and R&D Support: Quiet but Transformational
Strengthening the drug regulator and biopharma R&D may lack headline appeal, but it underpins global credibility. Regulatory maturity is what enabled South Korea and Ireland to transition from manufacturing bases to innovation hubs.
Advisory insight:
Indian pharma and med-tech companies that align early with global regulatory standards will find export pathways smoother and valuations stronger.
8. Tax and Duty Reliefs: Reducing Friction for Patients
Cuts in TCS on medical remittances and customs duties on cancer and rare-disease drugs, along with reduced personal import duties, directly lower patient friction. While fiscally modest, these measures improve affordability and signal patient-centric intent.
As Amartya Sen wrote in Development as Freedom: “Health is both a means and an end of development.” The budget reflects this duality.
Conclusion: A Platform Moment for Indian Healthcare
Union Budget 2026–27 does not merely increase healthcare spending—it re-architects the sector. By aligning innovation, workforce, infrastructure, regulation, and global engagement, it positions healthcare as a growth platform rather than a fiscal burden.
The opportunity now shifts to execution. As international experience shows, policy creates possibility—but strategy converts it into value.
Dr. Prahlada N.B
MBBS (JJMMC), MS (PGIMER, Chandigarh).
MBA in Healthcare & Hospital Management (BITS, Pilani),
Postgraduate Certificate in Technology Leadership and Innovation (MIT, USA)
Executive Programme in Strategic Management (IIM, Lucknow)
Senior Management Programme in Healthcare Management (IIM, Kozhikode)
Advanced Certificate in AI for Digital Health and Imaging Program (IISc, Bengaluru).
Senior Professor and former Head,
Department of ENT-Head & Neck Surgery, Skull Base Surgery, Cochlear Implant Surgery.
Basaveshwara Medical College & Hospital, Chitradurga, Karnataka, India.
My Vision: I don’t want to be a genius. I want to be a person with a bundle of experience.
My Mission: Help others achieve their life’s objectives in my presence or absence!
My Values: Creating value for others.
Leave a reply
















Leave a reply