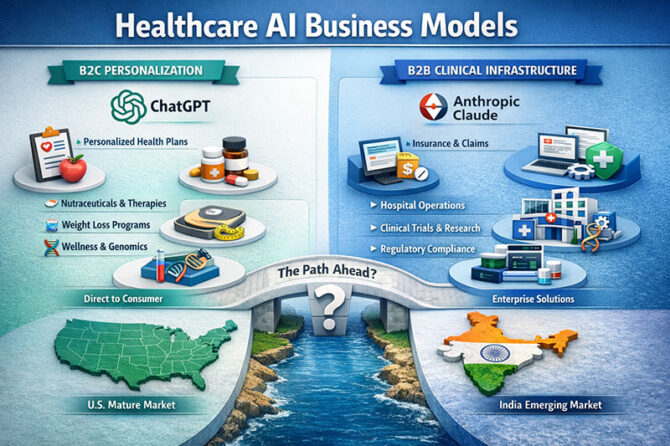
When people talk about AI in healthcare around the world, they frequently think of it as one big thing. But in reality, the field is quickly dividing into different business philosophies. Not only are there technical differences between ChatGPT and Anthropic Claude, but there are also two different ideas on how healthcare will be structured, paid for, and run in the next ten years. At its core, this split is between health management that focuses on the consumer over time and clinical and research infrastructure that is up to enterprise standards.
ChatGPT is mostly based on a B2C paradigm. Because of its conversational form, memory-driven continuity, and focus on keeping people engaged over time, it is best for long-term engagements with people rather than short-term clinical visits. It is assumed that health is not something that just happens in clinics or hospitals, but something that happens all the time in a person’s life. Chronic illness coaching, lifestyle changes, mental health assistance, preventive counselling, and continual analysis of personal health data are all things that this orientation naturally lends itself to. Over time, this kind of approach makes sense for businesses that want to offer personalized healthcare services like digital therapeutics, nutraceuticals, wellness subscriptions, weight-loss programs, and maybe even drug treatments that are tailored to each person’s behaviour and risk profile.
This way of doing things is in line with what is happening around the world, especially in the US, where consumer-driven healthcare markets are already well established. People often pay for genomic testing, health applications, wearable-driven analytics, and subscription-based wellness platforms out of their own pockets. In this case, AI is no longer a regulated therapeutic tool but a companion that is a part of everyday life. Eric Topol states in Deep Medicine (2019) that the best thing AI can do is “restore the human connection” by always being there for patients instead of just sometimes. This is what this vision is all about. In a B2C setting, though, that human connection is made through ongoing digital interaction and personalized data, with commercialization coming after trust and attention.
Anthropic Claude, on the other hand, has clearly gone the B2B route, especially in healthcare. Its early focus on following HIPAA rules is not just for show; it’s a strategic move. Claude’s main goal isn’t to talk to individual patients directly, but to fit into the workflows of institutions. It doesn’t just focus on the patient interface; it also adds value to provider operations and biomedical research at the same time. This layered approach recognizes that administrative problems, complicated rules, and slow data processing frequently have a bigger effect on healthcare outcomes than clinical understanding.
Claude’s use cases deal with some of the most common problems in modern healthcare systems in both clinical and administrative settings. Automating the maintenance of insurance databases and speeding up the processing of claims directly address the problems with the revenue cycle that affect both hospitals and insurers. Triage of patient queries based on severity, with smart routing to the right physicians, helps with access problems and keeps doctors from being too busy. When hospital and provider chatbots are powered by long-term clinical histories instead of pre-written answers, they can keep patients and make them happier without adding to the workload of staff. Atul Gawande wrote in The New Yorker in 2018 that the biggest problem with modern healthcare systems is the huge amount of paperwork that professionals have to do. These functions are quite similar to that.
Anthropic’s research layer is aimed toward pharmaceutical and life-sciences companies, which may be the most strategic move. The model is clearly at the high-value end of the healthcare value chain because it helps with writing clinical trial procedures, making sure that rules are followed, and analyzing massive genomic and multi-omic information. Even little improvements in efficiency can have huge effects on drug development delays, regulatory clearances, and research productivity. Claude is less vulnerable to the ups and downs of consumer markets and more closely tied to institutional demand by putting himself here.
In the US, this difference happens in a setting where the digital health infrastructure is quite well-developed. There are existing electronic health records, digitized insurance, regulatory standards like HIPAA, and established ways to get paid back. Because of this, the competition is no longer about basic skills, but about creating alliances and coming up with a go-to-market strategy. In this sense, Clayton Christensen’s The Innovator’s Prescription (2009) is still relevant. It says that healthcare innovation only works when technology fits with how people get paid and how things actually work. Anthropic’s “enterprise-first” strategy is a good example of this principle being followed with extraordinary discipline.
India, on the other hand, is a very different chessboard. There are a lot of health apps and wellness platforms for consumers, but workplace healthcare digitalization is still not very well connected. There are still problems with insurance coverage, electronic medical records, and interoperability standards. In this kind of setting, B2C health AI may grow quickly by avoiding problems with institutions, but B2B healthcare AI has a hard time without dependable data streams. Nandan Nilekani has said that platforms can only grow in a sustainable way when identity, trust, and transaction layers are all fixed at the same time. Enterprise AI usage will stay limited until India’s healthcare data and insurance systems are more advanced.
It’s evident what the strategic takeaway is. ChatGPT and other consumer-focused AI platforms are set up to take the lead in prevention, wellness, and individualized long-term care. Anthropic Claude and other enterprise-oriented platforms are better at changing clinical operations, insurance workflows, and biomedical research. Partnerships and execution will be key to success in the United States. In India, the biggest problem is creating the basic infrastructure that makes it possible for these kinds of businesses to work on a large scale. Healthcare AI is not just one market; it is a group of interconnected ecosystems. Choosing the incorrect one is not a technological mistake; it is a strategic one.
Dr. Prahlada N.B
MBBS (JJMMC), MS (PGIMER, Chandigarh).
MBA in Healthcare & Hospital Management (BITS, Pilani),
Postgraduate Certificate in Technology Leadership and Innovation (MIT, USA)
Executive Programme in Strategic Management (IIM, Lucknow)
Senior Management Programme in Healthcare Management (IIM, Kozhikode)
Advanced Certificate in AI for Digital Health and Imaging Program (IISc, Bengaluru).
Senior Professor and former Head,
Department of ENT-Head & Neck Surgery, Skull Base Surgery, Cochlear Implant Surgery.
Basaveshwara Medical College & Hospital, Chitradurga, Karnataka, India.
My Vision: I don’t want to be a genius. I want to be a person with a bundle of experience.
My Mission: Help others achieve their life’s objectives in my presence or absence!
My Values: Creating value for others.
Leave a reply
















Leave a reply