For decades, a familiar refrain echoed through boardrooms and tech forums: India excels at services, not systems. Deep technology, we were told, belongs to Silicon Valley. Advanced AI infrastructure? Built elsewhere. Deployed here.
That narrative is now being challenged.
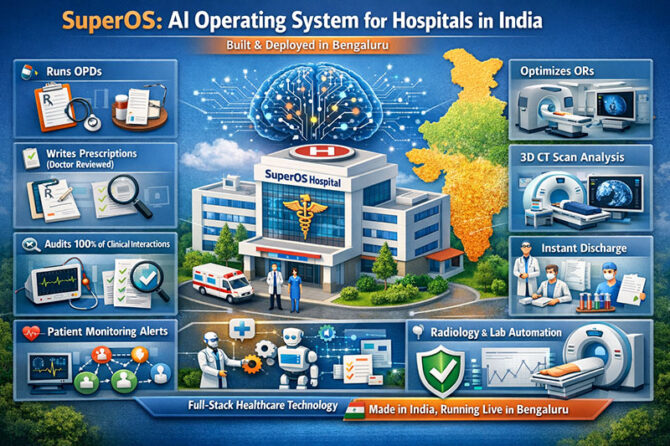
The launch of SuperOS — positioned as the world’s first AI Operating System running an entire hospital — marks a decisive shift in how we think about healthcare technology emerging from India. Not as peripheral software. Not as workflow augmentation. But as infrastructure.
From “AI Tools” to “AI Infrastructure”
Most AI deployments in healthcare globally have focused on narrow use cases: ambient scribes, billing optimization engines, clinical documentation support, and predictive dashboards. Even landmark systems such as IBM Watson Health, despite early promise, struggled when scaled into real-world clinical complexity. The lesson was clear: healthcare is not a single workflow problem; it is a systems problem.
SuperOS appears to approach healthcare differently — not as a tool layered onto hospitals, but as an operating layer embedded within them.
If reports are accurate, the system runs outpatient departments, drafts prescriptions (with physician review), audits clinical interactions in real time, optimizes operating room utilization, processes CT scans using 3D volumetric analysis, orchestrates AI agents and human teams, and enables instant discharge workflows. That scope moves AI from augmentation to governance.
As Stanford’s Fei-Fei Li once observed, “AI is not magic; it’s engineering.” The difference between a model and an operating system is precisely that engineering discipline — integration, control, reliability, and scale.
The Indian Healthcare Context
India’s healthcare challenges are systemic, not superficial. According to the World Health Organization, India faces a persistent shortage of radiologists relative to imaging demand. Operating theatre inefficiencies, discharge delays, and documentation variability compound cost pressures in both public and private systems. Alert fatigue — widely studied in U.S. hospitals — is equally relevant in Indian tertiary centers, where high patient volumes can overwhelm clinical teams.
An AI operating system trained on Indian clinical data and deployed in a live Bengaluru hospital addresses a long-standing structural gap: contextual intelligence. Western AI tools often fail in India because they are not trained on Indian epidemiology, prescribing patterns, workflows, or resource constraints.
As Nandan Nilekani has frequently argued in the context of India Stack, “Technology becomes transformative when it is built as public infrastructure.” The same principle applies to hospitals. Healthcare AI must operate at infrastructure depth, not cosmetic surface.
Global Parallels and Divergences
Internationally, AI integration has been incremental. Mayo Clinic and Cleveland Clinic have piloted AI-assisted diagnostics and workflow enhancements. In the UK, the NHS has explored predictive analytics for patient flow. However, few systems claim to orchestrate end-to-end hospital operations under a unified AI layer.
China has invested heavily in AI-enabled imaging diagnostics, while U.S. startups focus on specialty-specific automation. Yet most of these remain modular. The ambition to “run the hospital” — to coordinate clinical, operational, and administrative layers in real time — represents a more integrated vision.
This echoes Clayton Christensen’s theory of disruptive innovation: transformation occurs not by improving existing workflows incrementally, but by redefining the architecture of delivery itself.
Deep Tech from India
India’s reputation as a services powerhouse was earned through IT outsourcing and enterprise software implementation. But deep tech requires control over both domain and infrastructure. A company that designs, builds, and operates hospitals — while simultaneously engineering the technology stack — occupies a rare full-stack position.
In effect, healthcare becomes both laboratory and production environment.
The uncomfortable truth is that many global “AI in healthcare” products are, as critics note, digital polish — impressive dashboards that leave systemic bottlenecks untouched. Radiologist shortages persist. OR scheduling inefficiencies remain. Clinical audits are retrospective rather than real time.
If an AI operating system can audit 100% of clinical interactions in real time, optimize operating theatres algorithmically, and provide contextual alerts instead of noisy notifications, then it addresses structural deficits — not cosmetic inefficiencies.
Governance, Safety, and Ethics
However, ambition must be matched by safeguards. The history of AI in medicine underscores the importance of physician oversight, explainability, and data governance. The World Medical Association’s ethical guidance and the European Commission’s AI Act both stress transparency and accountability in clinical AI deployment.
A system that drafts prescriptions must remain doctor-reviewed. Real-time auditing must respect patient privacy and regulatory compliance. Infrastructure-level AI demands infrastructure-level ethics.
As Atul Gawande has written, “Better is possible.” But better requires disciplined implementation.
What This Means for India — and the World
If India can design and deploy an AI operating system that genuinely runs a hospital in real-world conditions — not a sandbox — it alters the global innovation map. It signals that deep AI products need not originate exclusively from Silicon Valley. They can emerge from Bengaluru, trained on Indian data, solving Indian constraints — and then scale outward.
The implications are profound:
- AI becomes embedded governance, not peripheral assistance.
- Clinical audits shift from retrospective sampling to continuous assurance.
- Discharge chaos converts into orchestrated throughput.
- Resource shortages are mitigated through algorithmic optimization.
Healthcare does not need more fragmented SaaS tools. It needs systems.
If SuperOS represents true infrastructure AI — not marketing gloss — then the debate over India’s deep tech capability is not merely academic. It is operational.
And once infrastructure shifts, narratives follow.
The real question is no longer whether India can build deep AI systems.
It is how quickly the rest of the world will adapt to that reality.
Dr. Prahlada N.B
MBBS (JJMMC), MS (PGIMER, Chandigarh).
MBA in Healthcare & Hospital Management (BITS, Pilani),
Postgraduate Certificate in Technology Leadership and Innovation (MIT, USA)
Executive Programme in Strategic Management (IIM, Lucknow)
Senior Management Programme in Healthcare Management (IIM, Kozhikode)
Advanced Certificate in AI for Digital Health and Imaging Program (IISc, Bengaluru).
Senior Professor and former Head,
Department of ENT-Head & Neck Surgery, Skull Base Surgery, Cochlear Implant Surgery.
Basaveshwara Medical College & Hospital, Chitradurga, Karnataka, India.
My Vision: I don’t want to be a genius. I want to be a person with a bundle of experience.
My Mission: Help others achieve their life’s objectives in my presence or absence!
My Values: Creating value for others.
Leave a reply
















Leave a reply