
Small and medium hospitals in the current healthcare landscape experience increasing pressure to provide high-quality care while enhancing financial viability. Of the many levers available at the administration’s command, the least thought-about but essential tool is the average length of stay, or ALOS. ALOS, being more than the clinician’s statistical abstraction, significantly affects the efficiency of the hospital, satisfaction of the patients, as well as the finances. For small hospitals, in which every bed spot is a valuable asset, reducing ALOS can go a long way in improving the provision of care as well as income.
The ALOS is the average of hospital days from the time of admission until discharge. Though one would believe that longer stays are correlated with better care, this is rarely the case. Long stays are frequently the consequence of inefficient practices that aren’t clinically driven, like slow diagnostics, slow discharge, insurance pre-authorization, or inefficient coordination across diverse departments. These small-appeared inefficiencies clog capacity, slow the turnover of patients, and prevent hospitals from utilizing their limited infrastructures effectively. Reducing ALOS without compromising clinical quality lets hospitals bring in more patients, through the more efficient use of current assets, and significantly boost their Average Revenue Per Occupied Bed (ARPOB).
The financial benefit of reducing ALOS is especially evident when you look at the way throughput and case mix meet. Take the example of the 30-bed hospital ward with ARPOB that moves from ₹10,000 for typical cases to ₹25,000 for high-complexity cases. By reducing ALOS from 4.5 days to only 3.5 days, the hospital can bring in an additional 28% percent of patients annually. The added capacity also translates into the administrators being able to bring in more high-value patients. If only 20 percent of the new admits end up in the more pricey ARPOB bracket of ₹25,000, the hospital is able to bring in an additional ₹1 crore plus per year in revenue. The point is that this expansion occurs with no added infrastructure or number of beds. For small hospitals, which often exist along thin margins, that can be nothing short of dramatic.
ALOS can be reduced using conscious strategies. Perhaps the most effective is the application of standardized clinical pathways. Standardization reduces variation in the provision of care, ensures that evidence-based techniques are always applied, and reduces unnecessary wait. For example, the application of a standard pathway in the chest pain management of patients includes cardiological review, diagnostic imaging, and the making of intervention choices within an established timeframe. Not only is this safer from the perspective of the patient but the preventable wait is reduced, and hospital lengths of stay are shorter and more consistent. For small hospitals with limited means, the application of this kind of protocol allows the benefits of using a structured methodology that at the same time optimizes care while optimizing efficiency.
Discharge planning is another area that significantly impacts ALOS. Hospitals often delay discharges purely because pharmacy clearance, billing, or family instruction is not initiated until discharge day. Institutionalizing the practice that discharge readiness is reviewed from the time of hospital admission will enable hospitals systematize discharge. Hospitals that strictly observe the policy of discharging up to noon typically experience remarkable fluctuations in throughput. Earlier in the day, hospital beds becoming empty become available as new admissions are admitted with no wait. The effect is that more time is spent with occupied beds, faster turnover, and better financial results, all of which are critical when small hospitals compete with large corporate healthcare providers.
Turnaround time in diagnosis also adds directly to longer hospital stays. If the report of a CT scan is submitted to the responsible doctor six hours after finalizing instead of two, then the hospital can keep the patient half a day longer than necessary. Spending money on faster reporting systems, point-of-care testing, or tele-radiology services can cut down significantly on delays. Though cutting just a few hours per case may seem trivial, the cumulative effect in scores of cases per week translates into enormous efficiency gains and improved ARPOB. For small hospitals with small diagnostic units, focusing on efficiency and promptness in reporting is one of the least expensive measures that can decrease ALOS.
Insurance-related processes like pre-authorization before discharge are another clandestine chokepoint. Routine is that the clinically well discharge-eligible patient will end up being admitted for an extra day due to the slow approval of the insurer. Such days earn no revenue but consume valuable bed capacity. Installing the special insurance assistance desk, the automation of pre-approval requests, and the preservation of ongoing payer contact will take care of the same. Getting rid of the non-revenue bed days benefits the hospitals in cash flow terms as well as creates more new bed capacity.
Of paramount importance is the clarification that ALOS reduction is definitely not premature discharge. The focus is rather on the delivery of timely, appropriate, and coordinated care that avoids unwarranted stays. Briefer hospitalizations, when clinically appropriate, are accompanied by reduced out-of-pocket costs among patients, reduced hospital-acquired infection hazards, and swift normal-activity return. For the hospital, this translates into improved ARPOB, improved bed use, and improved reputation. For small hospitals that depend largely on trust among patients and community referrals, the pairing of better results with efficiency is especially invaluable.
Reasons for Extended ALOS and Solutions:
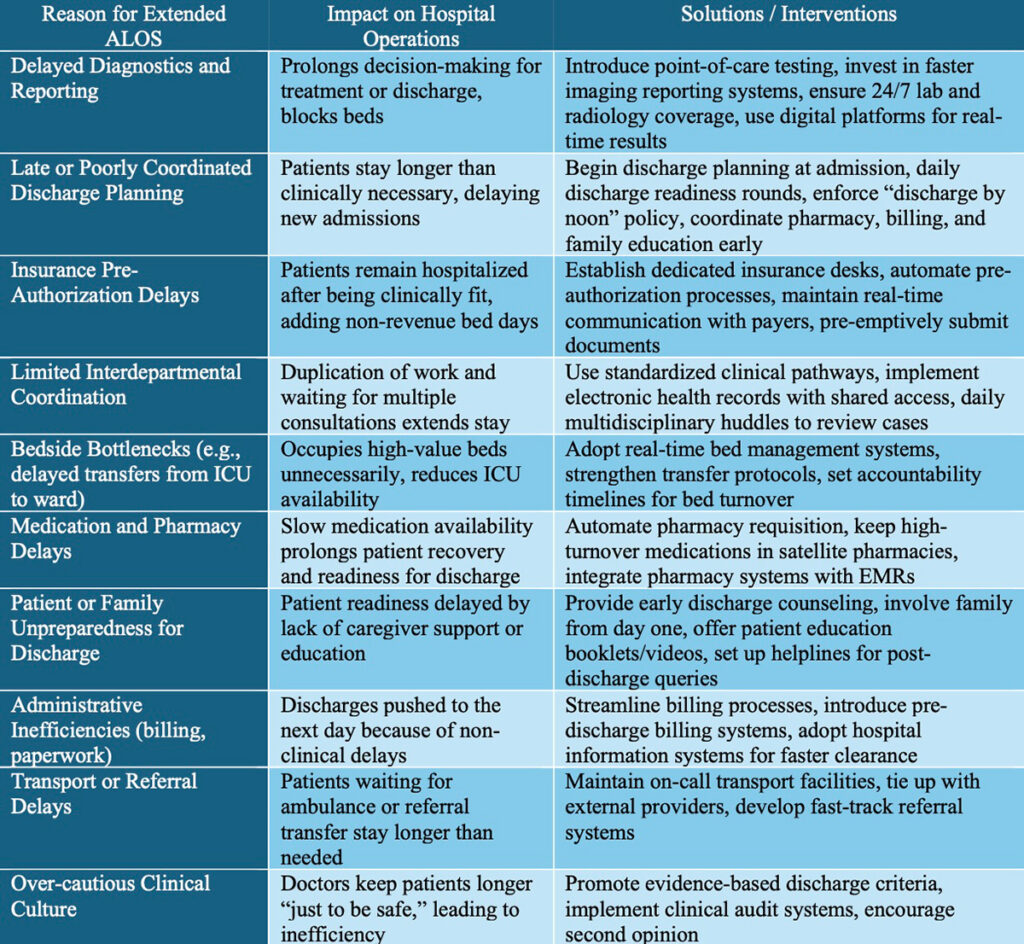
For small hospitals competing against the big hospitals in the marketplace, shortening ALOS needs to be considered strategically. Through the audit of prevailing ALOS trends, the detection of inefficiencies, and the implementation of controlled enhancements in pathways, discharge planning, diagnostics, and insurance coordination, hospitals are enabled to liberate notable dormant capacity. Those advantages go beyond the economic expansion. The patients get timely care better, the staff works within the more stable workforce, and the hospital solidifies its reputation within the community.
At last, reducing ALOS is one of the strongest underleveraged strategies for small hospitals. Alone among the strategies, reducing ALOS aligns both clinical excellence and economic survivability. By being more efficient in ways that don’t translate into the quality of care given, the hospital can bring in more patients, use available assets more effectively, and increase ARPOB—all without investing in new physical plant. For small- and medium-size hospitals that face an environment both intensely competitive and scarce in physical assets, an orientation toward reducing ALOS may be the only means of survival as well as long-term thriving.
Dr. Prahlada N.B
MBBS (JJMMC), MS (PGIMER, Chandigarh).
MBA in Healthcare & Hospital Management (BITS, Pilani),
Postgraduate Certificate in Technology Leadership and Innovation (MIT, USA)
Executive Programme in Strategic Management (IIM, Lucknow)
Senior Management Programme in Healthcare Management (IIM, Kozhikode)
Advanced Certificate in AI for Digital Health and Imaging Program (IISc, Bengaluru).
Senior Professor and former Head,
Department of ENT-Head & Neck Surgery, Skull Base Surgery, Cochlear Implant Surgery.
Basaveshwara Medical College & Hospital, Chitradurga, Karnataka, India.
My Vision: I don’t want to be a genius. I want to be a person with a bundle of experience.
My Mission: Help others achieve their life’s objectives in my presence or absence!
My Values: Creating value for others.
Leave a reply
















Dear Dr. Prahlada N. B Sir,
Thanks for another insightful post on the survival and flourishing of smaller hospitals in the era of corporate hospitals. Your strategies for reducing Average Length of Stay (ALOS) and increasing Average Revenue Per Occupied Bed (ARPOB) are truly beneficial for smaller hospitals.
As a pediatrician, I've implemented similar strategies to optimize patient care and hospital efficiency. For instance, I admit patients for shorter periods, typically just one day, and recommend continuing IV antibiotics at home or elsewhere, which aligns with your suggestions. This approach not only reduces ALOS but also enhances ARPOB, ultimately benefiting both patients and the hospital.
*Key Takeaways:*
– *Standardized Clinical Pathways*: Implementing evidence-based pathways can streamline care, reduce unnecessary waits, and improve patient outcomes.
– *Efficient Discharge Planning*: Reviewing discharge readiness from admission and discharging patients by noon can significantly improve bed turnover and hospital efficiency.
– *Prompt Diagnostic Reporting*: Investing in faster reporting systems or tele-radiology services can minimize delays and enhance patient care.
By adopting these strategies, smaller hospitals can improve patient satisfaction, increase revenue, and maintain a competitive edge in the healthcare landscape. Your article provides valuable insights and practical advice for healthcare professionals like myself, and I appreciate your expertise in this area.
Thank you for sharing your knowledge and experience.
Reply